PAEDIATRIC CUTANEOUS MASTOCYTOSIS : REPORT OF 3 CASES
*Dr. Ann Rose Thomas (Junior resident) , Dr. Sheethal B (Senior resident), Dr. Jayalakshmi P.L(Associate professor) , Dr. Sankar S(Professor and HOD)
Department of Pathology, Govt. Medical college Kottayam, Kerala, India
Received Date: 04/04/2022; Published Date: 22/04/2022.
*Corresponding author: Dr. Ann Rose Thomas ,Department of Pathology, Govt. Medical college Kottayam, Kerala, India
Mail : annrosethomas1@gmail.com
DOI: 10.55920/IJCIMR.2022.02.001064
Abstract
Mastocytosis occurs due to clonal, neoplastic proliferation of mast cells that accumulate in one or more organ systems. It is characterized by an abnormal mast cell infiltrates1 . It can be divided into cutaneous and systemic Mastocytosis. Mast cell infiltrates remain confined to skin in cutaneous Mastocytosis. Urticaria pigmentosa / Maculopapular cutaneous Mastocytosis , Diffuse cutaneous Mastocytosis and mastocytoma of skin are the 3 variants of cutaneous Mastocytosis. Systemic mastocytosis is characterized by the involvement of atleast one extracutaneous organ with or without evidence of skin lesions. This paper describes 3 cases of paediatric cutaneous mastocytosis.
Key Words : Cutaneous mastocytosis, Mast cell , Pediatric
Introduction
Mastocytosis is characterized by an abnormal mast cell infiltrates. It can occur at any age. Severity of this disease ranges from fleetingly benign to aggressively malignant contitions. Cutaneous mastocytosis is most common in children. About 50% of affected children develop typical skin lesions before the age of 6 months. In cutaneous mastocytosis, mast cells infiltrates remain confined to skin, whereas systemic mastocytosis is characterized by involvement of at least one extra cutaneous organ with or without evidence of skin lesion.
CASE REPORTS
CASE 1
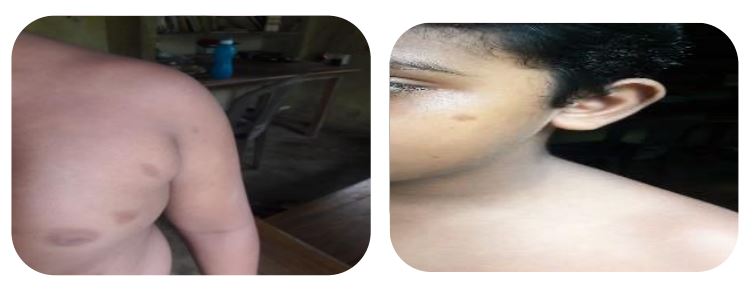
A 9 year old male child presented with generalized eruption of multiple hyperpigmented maculopapular lesions on face , trunk and extremities of 5 year duration. There was also history of generalized urticarial flushing. Growth and development status of the child is normal. On examination there were multiple sharply defined macules and papules over trunk, face and extremities. On stroking the individual lesions, there was formation of wheal and flare .
Darier’s sign was positive, Systemic examinations were normal and routine blood examination, liver and renal function test were within normal limits. Peripheral blood smear was normal. No abnormality detected in abdominal sonography. Histopathological examination showed skin with epidermis showing increased basal layer pigmentation, with mononuclear infiltrates in dermis. Toluidine blue stain showed multiple perivascular mast cells with metachromatic granules (purple colored granules ) in the dermis.
CASE 2
2 month old male infant presented with complaints of brownish to purplish macules and papules all over the body and excessive crying. Perinatal period was uneventful and exclusively breast fed with immunization up to date. No history of any drug intake. On examination there is diffuse macules and papules all over the body, chiefly distributed over the trunk associated with hyper and hypopigmentation. No hepatosplenomegaly or lymphadenopathy.
Darier’s sign was Positive, Systemic examination was normal. Routine blood examination and serum biochemistry are within normal limits. Peripheral smear showed mild thrombocytosis No abnormality detected in abdominal sonography. H&E –Diffuse infiltration of round to spindle shaped mononuclear cells in dermis. Toluidine blue and giemsa stain showed metachromatic granules in mast cells. Immunohistochemistry – Mast cells showed strong positivity with CD117 . CD1a and CD 68 were negative.
CASE3
7 month old male baby presented with hyper pigmented raised lesion and a few discrete hyper pigmented and skin colored small papules on left ankle for 4 months. History of scratching and occasional oozing of pus from the lesion present . Child is developmentally normal. On examination, Single hyperkeratotic crusted plaque 2x1 cm over left ankle and a few small hyper pigmented and skin colored papules seen. No other similar lesions over the body.
CD117
Darier’s sign – Positive. Systemic examination was normal. Routine blood investigations and serum biochemistry are within normal limits. Peripheral blood smear within normal limits. Abdominal Sonography – No abnormality detected. Histopathology - Diffuse infiltration of round to oval shaped cells in superficial and deep dermis. Eosinophils seen interspersed between mononuclear cells. Metachromatic granules in Mast cells demonstrated with Toluidene blue stain Immunohistochemistry – CD117, CD1a and CD68 were negative
Discussion
Mastocytosis is first described by Nettleship and Tay in 1869 and later due to the appearance like urticarial, The term Urticaria pigmentosa was coined by Sangster in 1878. Classification of Mastocytosis variants2 (WHO classification of tumors of Hematopoietic and lymphoid tissue-2017)
Cutaneous Mastocytosis
- Urticaria Pigmentosa or Maculopapular cutaneous mastocytosis.
- Diffuse cutaneous mastocytosis
- Mastocytoma of skin
Systemic mastocytosis
- Indolent systemic mastocytosis
- Smouldering systemic mastocytosis
- Systemic mastocytosis with an associated hematological neoplasm.
- Aggressive systemic mastocytosis
- Mast cell leukemia
Mast cell sarcoma
Mastocytosis can occur at any age. There is no gender difference. Cutaneous mastocytosis is most common in children and can be present at birth. About 50% of affected children develop typical skin lesions before the age of 6 months. There is a tendency of regression with age. In cutaneous mastocytosis, mast cells infiltrates remain confined to skin, whereas systemic mastocytosis is characterized by involvement of at least one extra cutaneous organ with or without evidence of skin lesion. About 10% of patients with proven systemic mastocytosis do not have skin lesions.3 The lesion of all forms may urticate when stroked (Dariers sign) and most show intra epidermal accumulation of melanin pigment. Despite variety of clinical presentation, The common picture is diffuse infiltration of mast cells in the dermis. Urticaria pigmentosa is the most common form of cutaneous mastocytosis, Lesions are larger, fewer and more papular. Diffuse cutaneous mastocytosis is less common than urticarial pigmentosa and present almost exclusively in childhood. Mastocytoma of skin, typically occurs as a single lesion, almost exclusively in children. In adult patients there is a genetic inactivation mutation of growth factor receptor C-kit and this mutation may be absent in pediatric cases and which is not associated with prognosis.4 The diagnosis is mainly clinical. Serum tryptase levels correlates with severity. Histopathological examination is essential for a definite diagnosis, The mast cells are usually oval or spindle shaped with granules that stain metachromatically with toluidine blue. They are also well demonstrated by Giemsa, tryptase or chloroacetate esterase in formalin fixed biopsies. Distinguishing between cutaneous and systemic mastocytosis in patients presenting with skin lesions depends on further investigation, including bone marrow biopsy and blood tryptase measurements.3 Prognosis depends on age, severity and clinical subtypes5 . Treatment is symptomatic with antihistamines and avoidance of drugs which may stimulate the mast cell to degranulate6 . Topical steroids also useful.
FOLLOW UP
All the 3 children showed good response to antihistamines and topical steroids, and currently doing well
CONCLUSIONS
Mastocytosis is characterized by an abnormal mast cell infiltrates. The diagnosis of cutaneous mastocytosis requires the demonstration of typical clinical findings and Histological proof of abnormal mast cell infiltration of dermis. In cutaneous mastocytosis. There is no evidence of systemic involvement in the bone marrow or any other organ. Patients with cutaneous mastocytosis without systemic involvement have a good prognosis. Careful long term follow up is essential for the early detection of systemic involvement.
Reference
- James W. Patterson. Weedon’s skin pathology. 5th ed. ELSEVIER; 2021. 155–210 p.
- Horny H P, Daniel A Arber,Steven H Swerdlow, editor. WHO classification of tumors of Hematopoietic and lymphoid tissue-2017. 4th ed. Lyon; 62–69 p.
- Arthur Rook, Darrell Wilkinson, John Ebling. Rook’s Text book of Dermatology. 9th ed. Vol. 2. WILEY Blackwell; 2016. 50.1-50.56.
- Hussain SH. Pediatric mastocytosis. Current Opinion in Pediatrics. 2020 Aug;32(4):531– 538.
- Heide R, Beishuizen A, De Groot H, Den Hollander JC, Van Doormaal JJ, De Monchy JGR, et al. Mastocytosis in children: a protocol for management. Pediatr Dermatol. 2008 Aug;25(4):493–500.
- Chatterjee S, Mukherjee S, Sinha M. Diffuse cutaneous mastocytosis in an infant. Indian J Paediatr Dermatol. 2016;17(3):209