Review Article
Nutrition during pregnancy in the Eritrean context
Lidia Ghirmai*
*Midwifery Unit, Department of Nursing, Orotta College of medicine and health sciences, Asmara, Eritrea.
Received Date: 15/10/2022; Published Date: 31/10/2022.
*Corresponding author: *Lidia Ghirmai, Midwifery Unit, Department of Nursing, Orotta College of Medicine and Health Sciences, Asmara, Eritrea.
DOI: 10.55920/IJCIMR.2022.03.001117
Introduction
A woman’s nutritional status prior to and during pregnancy influences the baby’s and her own health. A woman's nutritional status should be assessed preconceptionally with the goal of optimizing maternal, fetal, and infant health. Pregnancy-related dietary changes should begin prior to conception, with appropriate modifications across pregnancy and during lactation. During pregnancy, women should eat an extra meal per day (in their second and third trimester, no extra needed in the first one) as well as reduce physical workload during the final months of pregnancy in order to gain enough weight. The recommended intake is adding 0, 340, and 452 kcal/day to the estimated nonpregnant energy requirements in the first, second, and third trimesters, respectively.
Why do We Avoid Malnutrition?
Hazards of maternal malnutrition
Malnutrition should be avoided because it has the following hazards on the maternal and fetal health.
How do women become malnourished?
- Have been malnourished in childhood.
- Have not eaten enough food to cover energy needs.
- Have a heavy physical workload.
- Do not eat enough of different types of foods, existing food taboos for pregnant or lactating women.
- Do not get extra food when pregnant and/or lactating.
- Have babies when they are young (teenage pregnancy/delivery) or poorly spaced children.
Meanings of Healthy Diet
Healthy diet incorporates many things. Amongst them are:-
- Eating well
- Eating a variety of foods
- Add extra meal
- Talking to women about food
- Eating well with little money
Eating well: Eating well means eating a variety of healthy foods and also eating enough food. This combination helps a pregnant woman and her baby stay healthy and strong because it:
- Helps a woman resist illness during her pregnancy and after the birth
- Keeps a woman’s teeth and bones strong
- Gives a woman strength to work
- Helps the baby grow well in the mother’s uterus
- Helps a mother recover her strength quickly after the birth so that she has all the energy to look after the baby
- Supports the production of plenty of good quality breast milk to nourish the baby
Eating a variety of foods: It is important for pregnant women (like everyone else) to eat different kinds of food: A meal should have at least one food from each of the following food groups:
- Energy-giving
- Body-building
- Protective food and water
This can be specifically explained in the following ways:-
- Main foods (carbohydrates)
- Grow foods (proteins)
- Glow foods (vitamins and minerals)
- Go foods (fats, oils and sugar), along with plenty of fluids.
Add extra meal: Pregnant women and women who are breastfeeding need to eat more than usual by eating small and frequent meals in addition to the usual three servings per day practiced during her non pregnant state. The added extra meal gives them enough energy and strength, and helps their babies grow. They need to increase their usual food intake by at least 200 calories per day, or even more than this if they were underweight before they became pregnant.
There are many ways to increase daily food intake by this amount: for example, one more serving of maize porridge and 12 ground nuts a day would meet this additional requirement. Some pregnant women feel nauseated and do not want to eat. But pregnant women need to eat enough even when they do not feel well. Simple foods like Injera or rice can be easier for these women to eat. For women who suffer from nausea, encourage small and frequent meals.
Talking to women about food: Every second or minute of your contact with a pregnant women matters. So, when you see her during ANC visit, try to find out what the mother is eating. If pregnant women are to have a better chance of staying healthy, to have normal births and to have a healthy baby, they should start eating healthier foods earlier. You can enquire about she usually eats and how much. You can simply ask her what she consumed the day before. Based on that, tell her the necessary modification of what she needs to do, be sure to tell her what is healthy about what she eats, reinforce the positive efforts she is making to eat well. Then, accordingly make a suggestion for how she could eat better.
Eating well with little money: Remember that education about food is not enough on its own to change eating behavior. Even if a woman knows the best foods for health, she may not eat them. Many families cannot afford to buy enough food or a wide variety of foods. Some women may simply not like the taste of some healthy foods. To help a woman eat better, suggest healthy foods that she can afford and will choose to eat. The biggest cause of poor nutrition is poverty. A very poor family can eat better by spending money wisely and not wasting what little they have.
Here are some ideas that families can use to eat better with little money.
Legumes: Beans, peas and lentils belong to a family of vegetables called legumes. All legumes have a lot of protein and vitamins, and they usually do not cost much. They have even more vitamins if they are sprouted (germinated) before being eaten. Planting legumes makes soil richer. Other crops such as maize will grow better in a field where legumes once grew.
Less expensive meats and animal products: Blood and organ meats like liver, heart and kidney have a lot of iron and may cost less than other meats. Fish and chicken are as healthy as other meats, and usually cost less - especially for a family that fishes or raises their own chickens. Eggs have a lot of protein, iron, and vitamin A. Eggs give more protein for less money than almost any other food.
Whole grains: Grains like taff, wheat, rice and corn are more nutritious when they have not been refined (processed to take out the color). Taking out the color takes out healthy things too. White bread and white rice have fewer vitamins, minerals and proteins than brown bread or brown rice. Dark red taff and brown Injera are more nutritious than the light-colored ones.
Vegetables and fruits: When vegetables are boiled or steamed, some of the vitamins from the foods go into the cooking water. Use this water to make soups. The outside leaves of plants are usually thrown away, but sometimes they can be eaten.
Food Groups and Their Nutrients
Main foods (Carbohydrates): In most parts of the world, people eat one main food at each meal. This main food may be Injera, rice, maize, wheat, millet, or another low-cost, starchy food which is rich in carbohydrates. These foods give the body energy. But to grow and stay healthy, the body needs other types of food too.
Grow Foods (proteins): Grow foods contain protein, which is needed for the growth of muscles, bones, and strong blood. Everyone needs protein to be healthy and to grow. Some Grow foods that are high in proteins are:
- Legumes (beans, peas, soybeans, and lentils)
- Eggs
- Cheese, milk and yogurt
- Nuts and seeds
- Cereal, wheat, corn and rice
- Meat, poultry and fish.
- Meat, fish and cheese are nutritious foods but they can carry parasites or disease when they are eaten raw. Pregnant women should eat fish, meat or cheese only when it is well cooked or pasteurized.
Go foods (sugars and fats): Go foods contain sugars and fats, which give the body energy. Everyone needs these foods to be healthy. Some healthy Go foods that are high in sugars are: Fruits and Honey.
Some ‘Go foods’ that are high in fats are:
- Some nuts (e.g. peanuts) and some seeds (e.g. sunflower)
- Avocados, Vegetable oils, butter and margarine butter
- Fatty meat, Milk and cheese
- Eggs, Fish
These days, many people eat more sugars and fats than they need. That is because more people drink sugary soda pop, or eat foods that come from packages instead of foods made at home. These packaged, sugary and fatty foods are expensive and not as healthy as fresh products. They also damage the teeth. It is better to eat go foods that are natural, not packaged.
Glow foods (vitamins and minerals)
Glow foods contain vitamins and minerals, which help the body fight infection and keep the eyes, skin and bones healthy and strong. Vitamins and minerals are known as micronutrients because they are very small. Fruits and vegetables are high in vitamins and minerals. It is important for pregnant women to eat as many different fruits and vegetables as they can.
The four most important vitamins and minerals:
Pregnant and breastfeeding women need more of these five vitamins and minerals than other people do. They include iron, folic acid, calcium, iodine and vitamin A. They should try to get these vitamins and minerals every day.
Iron
In a typical singleton gestation, the maternal need for iron averages close to 1000 mg. Of this, 300 mg is for the fetus and placenta; 500 mg for maternal hemoglobin mass expansion; and 200 mg that is shed normally through the gut, urine and skin. The total amount of 1000 mg considerably exceeds the iron stores of most women and results in iron deficiency anemia unless iron supplementation is given.
Iron make blood healthy and prevents anemia. A pregnant woman needs a lot of iron to have enough energy, to prevent too much bleeding at the birth, and to make sure that the growing baby can form healthy blood and store iron for the first few months after birth. It is also important in the production of good breast milk.
These foods contain a lot of iron:
Taking iron pills
It can be difficult for a pregnant woman to get enough iron, even if she eats iron-rich foods every day. She should also take iron pills (or liquid iron drops) to prevent anemia. Daily oral iron and folic acid supplementation with 30 mg to 60 mg of elemental iron is recommended for pregnant women to prevent maternal anemia, puerperal sepsis, low birth weight, and preterm birth.
In the first and third trimesters, the Hb threshold for diagnosing anemia is 11 mg/dL; in the second trimester, the threshold is 10.5 mg/dL. If a woman is diagnosed with anemia during pregnancy, her daily elemental iron should be increased to 120 mg until her Hb concentration rises to normal (Hb 11 mg/L or higher).
Iron pills or drops can be obtained from pharmacies and health institutions, but throughout Eritrea iron pills are given routinely to pregnant women as part of focused antenatal care. She should receive 60 to 120 mg (milligrams) of ferrous sulphate once a day taken by mouth. She should begin the iron supplements as early as possible and continued throughout pregnancy
The iron pills may cause nausea, make it hard for the woman to pass stool (constipation), and her stool may turn black, but it is important for the woman to keep taking the iron pills because anemia can cause complications during pregnancy, during delivery, and after the baby is born. It is helpful for the woman to take the iron pill with a meal, drink plenty of fluids, and eat plenty of fruits and vegetables to avoid nausea and constipation. Tea and coffee reduce the ability to absorb iron and must be taken two hours after taking iron pills. The black color of the stool is a normal side-effect from the iron and is not harmful. To absorb more iron from vegetables (especially beans and peas), eat foods rich in vitamin C or citric acid containing foods at the same time (e.g. fruits, juice, tomatoes, fermented foods). Try to drink Tea and coffee between meals rather than when eating iron rich foods.
Intermittent oral iron and folic acid supplementation with 120 mg of elemental iron and 2800 µg (2.8 mg) of folic acid once weekly is recommended for pregnant women to improve maternal and neonatal outcomes if daily iron is not acceptable due to side effects, and in populations with an anemia prevalence among pregnant women of less than 20%.
Folate (folic acid)
All women, from the moment they plan to conceive until 12 weeks of gestation, should take a folic acid supplement.
Folic acid supplements during pregnancy is important for
- Normal development of the nervous system of the unborn baby (brain, spine and skull)
- Prevent birth defects/abnormalities the nervous system of the unborn baby.
- Prevents premature labor and delivery.
It is important if possible for a woman to get enough folic acid in her diet before she becomes pregnant and she should certainly do this in the first few months of pregnancy. Foods rich in folate that pregnant and breastfeeding women should try to eat every day include:
- Dark green, leafy vegetables
- Whole grains (brown rice, whole wheat)
- Meat (especially liver, kidney and other organ meats)
- Fish, Peas and beans
- Eggs, Sunflower, pumpkin and squash seeds (ኣባዕኸ)
- Mushrooms (ቓንጥሻ)
As well as eating as many of these foods as she can, all pregnant women should also take 400 mcg (micrograms) of folic acid tablets orally every day during pregnancy. She should be able to get these tablets from you as part of Focused Antenatal Care. A woman with a prior child with a neural-tube defect can reduce the 2-5% recurrence risk by more than 70% with daily 4-mg folic acid supplements the month before conception and during the first trimester.
Calcium
A growing baby needs a lot of calcium to make new bones, especially in the last few months of pregnancy. Women need calcium for strong bones and teeth. These foods contain a lot of calcium:
- Yellow vegetables (hard squash, yams)
- Milk, curd, yogurt and cheese
- Green, leafy vegetables
- Bone meal and egg shells
- Molasses and soybeans
- Sardines
Women can also get more calcium in these ways:
- Soak bones or eggshells in vinegar or lemon juice for a few hours. Then use the liquid to make soup or eat with other foods.
- Add lemon juice, vinegar or tomatoes when cooking bones.
- Grind eggshells into a fine powder and mix into food.
- Soak maize in lime (carbon ash) before cooking it.
- In populations with low dietary calcium intake, daily calcium supplementation (1.5– 2.0 g oral elemental calcium) is recommended for pregnant women to reduce the risk of pre-eclampsia.
Iodine
Iodine prevents goiter (swelling of the neck) and other problems in adults. Lack of iodine in a pregnant woman can cause her child to have cretinism, a disability that affects thinking and physical features. The easiest way to get enough iodine is to use iodized salt instead of regular salt. It is available in packet form labelled ‘Iodized salt’ in many market places.
- Women should drink plenty of clean water (6 to 8 glasses a day) and other healthy fluids every day. Fruit juices, animal milks and many herbal teas are all healthy fluids to drink.
Traditional foods during pregnancy
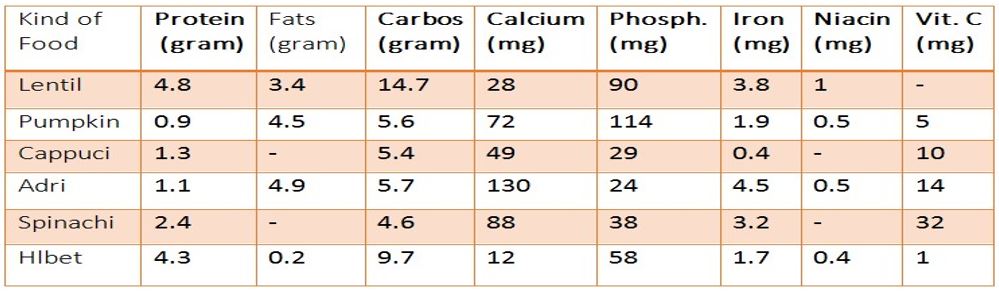
The following tables show the nutritional content of locally eaten foods. The content is expressed in grams or milligrams per 100 gram of the food kind.
Foods for breakfast
- As shown in the table, wheat loafs whether fermented or not, have high protein content than barley ones. Surprisingly, fermentation affects nutritional content of the food.
- It could be observed that unfermented wheat loaf has high fiber, calcium and Vit. C which decrease substantially when fermented. These nutrients are essential during pregnancy and should be benefited by pregnant mothers.
Hot drinks
- Milk is a good source of proteins and fats, though high carbohydrates content is attributed to spiced tea. Both milk and tea contain high amount of calcium which is main competitor of iron and thus should be avoided during iron supplementation as they decrease its absorption.
Lunch and dinner foods
- Though Injera contains good amount of protein, carbohydrates and some minerals, it lacks fat, vitamins (thiamin and riboflavin) and other minerals like zinc, copper, and selenium which are needed in trace amounts during pregnancy.
- Injera made of taff is a very good source of iron (especially red taff) which pregnant mothers have to benefit. Eating Injera made of sorghum and taff can be so beneficial provided one cannot prepare Injera from taff only.
- Tsebhi tlul sga, Tsebhi dnsh and Shiro contain high amount of Vit. A (1600, 1300 and 1200 ug respectively.) Taking these foods repeatedly, may not benefit pregnant mother.
- If prepared and cooked properly traditional foods do have needed nutrients but one type of food (tsebhi) of any kind cannot provide all the nutrients at the same time, hence additional dishes of vegetables or pulses are helpful in making the diet balanced.
Extra Tips
- The most abundant iron is found in “Abaeke”. If it is taken in the form of fluid, it has 341mg of iron per 100 grams of the fluid. Women who hate to drink “Abake” can benefit from it by fortifying their Injera flour with it. However, the potential iron content will be greatly reduced to about 16 grams. Drinking “Abaeke”. can be useful for women with anemia, and those with difficulty of taking iron supplements due to gastric complains.
- Chills, tomatoes and boiled potatoes have very high amount of Vit. C when raw rather than when prepared in food. So pregnant mothers can benefit from it by making tomato, Chillis, potatoes and onion salad during meals.
- Boiled eggs have greater protein, fat, calcium, iron and vitamin content than fried one
Ideal nutritional plan for a pregnant lady
- Breakfast: kicha or 2 bread with 2 fried eggs along with one cup of tea boiled with lemon/ kemem /and two tea spoons of sugar added to it.
- Lunch: taita with red sauce (tsebhi sga)
- One taita……500 grams
- Quarter kg of meat
- Two onions, one cup of oil, three tomatoes, one spoon pepper and salt
With
- Salad of 125 grams and 2 chills
- Add lemon to it or eat two oranges afterwards
- Dinner: taita with tsebhi shiro
- One taita….500 grams
- Two cups of shiro flour, two onions, two tomatoes, one cup of oil, two chills and salt With
- One cup of milk with two tea spoons of sugar added to it
Substances that may harm your baby
- Alcohol: Try not to drink alcohol during pregnancy. Alcohol crosses placenta and can lead to physical, growth and mental problems in some babies. It is especially important not to drink alcohol at the time of conception and during the first 3 months of pregnancy when the embryo is most vulnerable to the toxic effects of alcohol.
- Smoking: Try not to smoke during pregnancy or at least try to reduce smoking substantially. Mothers who are heavy smokers are at much higher risk of having low birth weight babies. Smoking can also be a cause of premature birth, miscarriage and stillbirth and may impair your child’s growth and development.
Remember: it is never too late to stop or at least reduce smoking or drinking. Your baby will benefit from each alcoholic drink or cigarette you give up!
- Caffeine: Effects of caffeine on the fetus are not well established yet. Tea, cocoa and cola-type drinks contain about the same amount of caffeine while coffee contains about twice as much caffeine. Try to limit your coffee intake to 3 cups a day.
Body Weight and Gestational Weight Gain
A commonly asked question is “how much weight should I gain?” A great deal of healthy individual variation exists. BMI is calculated by dividing weight in kg by height in m2. It is a simple way to assess body weight in relation to health, and is intended to promote acceptance of a wider range of healthy weights and variations in size.
Many evidences indicate that gestational weight gain, particularly during the second and third trimesters, is an important determinant of fetal growth. Institute of Medicine has put the “normal” weight gain in pregnancy according to the pre-pregnancy BMI of the women.
Reference
- Ashenafi Zelalem, Mulualem Endeshaw, Mamaru Ayenew, Solomon Shiferaw and Robel Yirgu
- (2017). Effect of Nutrition Education on Pregnancy Specific Nutrition Knowledge and
- Healthy Dietary Practice among Pregnant Women in Addis Ababa. OMICS
- International Clinics Mother Child Health 2017, Vol.14, Issue. 3 DOI: 10.4172/2090-7214.1000265
- Darnton HI. Nutrition counselling during pregnancy (2015). WHO
- Healthy Eating during Pregnancy and Breastfeeding: Booklet for mothers (2001): WHO
- Maternal Nutrition during Pregnancy and Lactation. In: LINKAGES (2004): Breastfeeding L,
- Related Complementary Feeding, and Maternal Nutrition Program, Group CSCaRCNW, Editors, Washington, DC.
- WHO on antenatal care for a positive pregnancy experience. 2016
- Up to date